Investigation and Treatment
Diagnosis
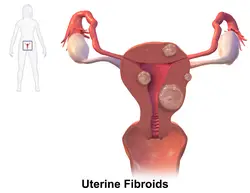
Physical examination and ultrasound are sufficient for diagnosing uterine fibroids in the majority of people. When ultrasound findings are inconclusive, magnetic resonance imaging (MRI) may be able to confirm the diagnosis of uterine fibroids in most cases. In addition, MRI can identify benign uterine fibroids with atypical imaging features and fibroids with variant growth patterns. MRI can also identify other uterine (e.g. adenomyosis, endometrial polyps, endometrial cancer) and extrauterine (e.g. benign and malignant ovarian tumors, endometriosis) disorders that may mimic the appearance of uterine fibroids and/or contribute to the patient’s symptoms.[38] However, a small proportion of uterine fibroids can mimic other malignant uterine tumors (e.g. leiomyosarcoma) on all available imaging modalities (e.g. ultrasound, CT, MRI and PET-CT).[38]
Malignant tumors of the uterine wall (e.g. leiomyosarcoma) are very rare. Findings suggestive of a malignant uterine tumor rather than a benign fibroid include, fast or unexpected growth (particularly after menopause), interruption/effacement of the endometrial stripe, lymph node enlargement, invasion of adjacent organs and metastases to distant organs (e.g. lung). MRI findings suggestive of a malignancy include nodular/ill-circumscribed tumor margins, intermediate/high T2-weighted signal intensity of the solid tumor components, regions with high signal T1-weighted sequences in keeping with subacute hemorrhage, fine/wispy enhancement of the solid parts of the tumor, and restricted diffusion on diffusion-weighted imaging (DWI).[38] A biopsy is rarely performed and if performed, is rarely diagnostic. Should there be an uncertain diagnosis after ultrasounds and MRI imaging, surgery is generally indicated.[39]
-
A very large (9 cm) fibroid of the uterus which is causing pelvic congestion syndrome as seen on CT
-
A very large (9 cm) fibroid of the uterus which is causing pelvic congestion syndrome as seen on ultrasound
-
A relatively large submucosal leiomyoma; it fills out the major part of the endometrial cavity.
-
A small uterine fibroid seen within the wall of the myometrium on a cross-sectional ultrasound view
-
Two calcified fibroids (in the uterus)
-
A subserosal uterine fibroid with a diameter of 5 centimeters
-
MRI image with multiple uterine leiomyomas
-
Giant leiomyomas almost filling the abdomen
-
Histopathology of uterine fibroids typically show smooth muscle in a whorled (fascicular) pattern.[40]
-
This variant of Van Gieson’s stain distinguishes muscle (yellow) from connective tissue (red).
-
Immunohistochemistry for β-catenin in uterine leiomyoma, which is negative as there is only staining of cytoplasm but not of cell nuclei.
Negative immunohistochemistry staining for β-catenin in cell nuclei is a consistent finding in uterine leiomyomas, and helps in distinguishing such tumors from β-catenin positive spindle cell tumors.[41]
Coexisting disorders
Fibroids that lead to heavy vaginal bleeding lead to anemia and iron deficiency. Due to pressure effects gastrointestinal problems such as constipation and bloatedness are possible. Compression of the ureter may lead to hydronephrosis. Fibroids may also present alongside endometriosis, which itself may cause infertility. Adenomyosis may be mistaken for or coexist with fibroids.
In very rare cases, malignant (cancerous) growths, leiomyosarcoma, of the myometrium can develop.[23] In extremely rare cases uterine fibroids may present as part or early symptom of the hereditary leiomyomatosis and renal cell cancer syndrome.
Treatment
Most fibroids do not require treatment unless they are causing symptoms. After menopause, fibroids shrink, and it is unusual for them to cause problems.
Uterine fibroids that cause symptoms can be treated by:
- medication to control symptoms (i.e., symptomatic management)
- medication aimed at shrinking tumors
- ultrasound fibroid destruction
- surgical removal of fibroids (myomectomy) or using heat to reduce size (radiofrequency ablation)
- surgical removal of the womb (hysterectomy)
- blocking the blood supply of fibroids (uterine artery embolization)
In those who have symptoms, uterine artery embolization and surgical options have similar outcomes with respect to satisfaction.[42]
For decades, a common approach to treating symptomatic fibroids was “either get a hysterectomy or wait until menopause diminishes the symptoms,” but minimally invasive (small incision) and noninvasive (no incision) options were often not offered.[43] Especially since the 2010s, minimally invasive and noninvasive options are increasingly being offered as they have advanced on their technological journey from being new and unusual to being common clinical practice.[43]
Medication
A number of medications may be used to control symptoms. Painkillers (NSAIDs) can be used to reduce painful menstrual periods. Oral contraceptive pills may be prescribed to reduce uterine bleeding and cramps.[11] Anemia may be treated with iron supplementation.
Levonorgestrel intrauterine devices are effective in limiting menstrual blood flow and improving other symptoms. Side effects are typically few as the levonorgestrel (a progestin) is released in low concentration locally.[44] While most levongestrel-IUD studies concentrated on treatment of women without fibroids a few reported good results specifically for women with fibroids including a substantial regression of fibroids.[45][46]
Cabergoline in a moderate and well-tolerated dose has been shown in two studies to shrink fibroids effectively. The mechanism of action responsible for how cabergoline shrinks fibroids is unclear.[45]
Ulipristal acetate is a synthetic selective progesterone receptor modulator (SPRM) that has tentative evidence to support its use for presurgical treatment of fibroids with low side-effects.[47] Long-term UPA-treated fibroids have shown volume reduction of about 70%.[48] In some cases UPA alone is used to relieve symptoms without surgery,[49] and to allow successful pregnancies without fibroid regrowth.[50] Indeed, in the tumor cells, the molecule blocks the cell proliferation, induces their apoptosis[51][52] and stimulates the remodeling of the extensive fibrosis by matrix metalloproteinases,[53] hence explaining the long-term benefit.[54] Yet, due to some rare but severe hepatic injuries after UPA treatment, the licence was suspended in 2020 in the EU[55] and voluntary removed in Canada.[56]
Danazol is an effective treatment to shrink fibroids and control symptoms. Its use is limited by unpleasant side effects. Mechanism of action is thought to be antiestrogenic effects. Recent experience indicates that safety and side effect profile can be improved by more cautious dosing.[45]
Gonadotropin-releasing hormone analogs cause temporary regression of fibroids by decreasing estrogen levels. Because of the limitations and side effects of this medication, it is rarely recommended other than for preoperative use to shrink the size of the fibroids and uterus before surgery. It is typically used for a maximum of six months or less because after longer use they could cause osteoporosis and other typically postmenopausal complications. The main side effects are transient postmenopausal symptoms. In many cases the fibroids will regrow after cessation of treatment, however, significant benefits may persist for much longer in some cases. Several variations are possible, such as GnRH agonists with add-back regimens intended to decrease the adverse effects of estrogen deficiency. Several add-back regimes are possible, tibolone, raloxifene, progestogens alone, estrogen alone, and combined estrogens and progestogens.[45]
Progesterone antagonists such as mifepristone have been tested, there is evidence that it relieves some symptoms and improves quality of life but because of adverse histological changes that have been observed in several trials it can not be currently recommended outside of research setting.[57] Fibroid growth has recurred after antiprogestin treatment was stopped.[36]
Aromatase inhibitors have been used experimentally to reduce fibroids. The effect is believed to be due partially by lowering systemic estrogen levels and partially by inhibiting locally overexpressed aromatase in fibroids.[45] However, fibroid growth has recurred after treatment was stopped.[36] Experience from experimental aromatase inhibitor treatment of endometriosis indicates that aromatase inhibitors might be particularly useful in combination with a progestogenic ovulation inhibitor.
Uterine artery
Uterine artery embolization (UAE) is a noninvasive procedure that blocks blood flow to fibroids, causing them to shrink.[58] Long-term outcomes with respect to how happy people are with the procedure are similar to that of surgery.[59] There is tentative evidence that traditional surgery may result in better fertility.[59] One review found that UAE doubles the future risk of miscarriage.[60] UAE also appears to require more repeat procedures than if surgery was done initially.[59] A person will usually recover from the procedure within a few days.
Uterine artery ligation, sometimes also laparoscopic occlusion of uterine arteries are minimally invasive methods to limit blood supply of the uterus by a small surgery that can be performed transvaginally or laparoscopically. The principal mechanism of action may be similar like in UAE but is easier to perform and fewer side effects are expected.[61][non-primary source needed][62][non-primary source needed]
The 2016 NICE (National Institute of Clinical Excellence – the non governmental public body that publishes guidelines in the use of health technologies and good clinical practice in the United Kingdom) guidelines state UAE/UFE can be offered to people with symptomatic fibroids (fibroids being usually >30mm in size). Patients should be informed that UAE and myomectomy (the surgical removal of fibroids) may potentially allow them to retain their fertility.[63]
Myomectomy
Myomectomy is a surgery to remove one or more fibroids. It is usually recommended when more conservative treatment options fail for patients who want fertility preserving surgery or who want to retain the uterus.[64]
There are three types of myomectomy:
- In a hysteroscopic myomectomy (also called transcervical resection), the fibroid can be removed by either the use of a resectoscope, an endoscopic instrument inserted through the vagina and cervix that can use high-frequency electrical energy to cut tissue, or a similar device.
- A laparoscopic myomectomy is done through a small incision near the navel. The physician uses a laparoscope and surgical instruments to remove the fibroids. Studies have suggested that laparoscopic myomectomy leads to lower morbidity rates and faster recovery than does laparotomic myomectomy.[65]
- A laparotomic myomectomy (also known as an open or abdominal myomectomy) is the most invasive surgical procedure to remove fibroids. The physician makes an incision in the abdominal wall and removes the fibroids from the uterus.
Laparoscopic myomectomy has less pain and shorter time in hospital than open surgery.[66] An analysis of 15,000 patients found that those who had myomectomy required fewer additional procedures to manage fibroids (including hysterectomies) over the next 5 years than those who had UAE.[67][68]
Hysterectomy
Hysterectomy was the classical method of treating fibroids. Although it is now recommended only as last option, fibroids are still the leading cause of hysterectomies in the US.
Endometrial ablation
Endometrial ablation can be used if the fibroids are only within the uterus and not intramural and relatively small. High failure and recurrence rates are expected in the presence of larger or intramural fibroids.
Other procedures
Radiofrequency ablation is a minimally invasive treatments for fibroids.[69] In this technique the fibroid is shrunk by inserting a needle-like device into the fibroid through the abdomen and heating it with radio-frequency (RF) electrical energy to cause necrosis of cells. The treatment is a potential option for people who have fibroids, have completed child-bearing and want to avoid a hysterectomy.
Magnetic resonance guided focused ultrasound, is a non-invasive intervention (requiring no incision) that uses high intensity focused ultrasound waves to destroy tissue in combination with magnetic resonance imaging (MRI), which guides and monitors the treatment. During the procedure, delivery of focused ultrasound energy is guided and controlled using MR thermal imaging.[70] Patients who have symptomatic fibroids, who desire a non-invasive treatment option and who do not have contraindications for MRI are candidates for MRgFUS. About 60% of patients qualify. It is an outpatient procedure and takes one to three hours depending on the size of the fibroids. It is safe and about 75% effective.[71] Symptomatic improvement is sustained for two plus years.[72] Need for additional treatment varies from 16 to 20% and is largely dependent on the amount of fibroid that can be safely ablated; the higher the ablated volume, the lower the re-treatment rate.[73] There are currently no randomized trial between MRgFUS and UAE. A multi-center trial is underway to investigate the efficacy of MRgFUS vs. UAE.
Prognosis
About 1 out of 1,000 lesions are or become malignant, typically as a leiomyosarcoma on histology.[11] A sign that a lesion may be malignant is growth after menopause.[11] There is no consensus among pathologists regarding the transformation of leiomyoma into a sarcoma.
Metastasis
There are a number of rare conditions in which fibroids metastasize, for example extrauterine fibroids. They still grow in a benign fashion, but can be dangerous depending on their location.[29]
Epidemiology
About 20% to 80% of women develop fibroids by the age of 50.[13][1] Globally in 2013 it was estimated that 171 million women were affected.[6] They are typically found during the middle and later reproductive years.[1] After menopause they usually decrease in size.[1] Surgery to remove uterine fibroids occurs more frequently in women in “higher social classes”.[13] Adolescents develop uterine fibroids much less frequently than older women.[8] Up to 50% of people with uterine fibroids have no symptoms. The prevalence of uterine fibroids among teenagers is 0.4%.[8]
Europe
The incidence of uterine fibroids in Europe is thought to be lower than the incidence in the US.[13]
United States
Eighty percent of African American women will develop benign uterine fibroid tumors by their late 40s, according to the National Institute of Environmental Health Sciences.[74] African American women are two to three times more likely to get fibroids than Caucasian women.[13][14][75] In African American women fibroids seem to occur at a younger age, grow more quickly, and are more likely to cause symptoms.[76] This leads to higher rates of surgery for African Americans, both myomectomy, and hysterectomy.[77] Increased risk of fibroids in African Americans causes them to fare worse in in-vitro fertility treatments and raises their risk of premature births and delivery by Caesarean section.[77]
It is unclear why fibroids are more common in African American women. Some studies suggest that black women who are obese and who have high blood pressure are more likely to have fibroids.[77] Other suggested causes include the tendency of African American women to consume food with less than the daily requirements for vitamin D.[13]
Related legislation
United States
The 2005 S.1289 bill was read twice and referred to the committee on Health, Labor, and Pensions but never passed for a Senate or House vote; the proposed Uterine Fibroid Research and Education Act of 2005 mentioned that $5 billion is spent annually on hysterectomy surgeries each year, which affect 22% of African Americans and 7% of Caucasian women. The bill also called for more funding for research and educational purposes. It also states that of the $28 billion issued to NIH, $5 million was allocated for uterine fibroids in 2004.[78]








![Histopathology of uterine fibroids typically show smooth muscle in a whorled (fascicular) pattern.[40]](https://upload.wikimedia.org/wikipedia/commons/thumb/7/79/Histopathology_of_uterine_leiomyoma.jpg/120px-Histopathology_of_uterine_leiomyoma.jpg)

