Definition: Non-cancerous enlargement of prostate gland causing urinary issues.
Causes: Ageing, hormonal imbalance (testosterone & DHT).
Symptoms: Frequent urination, dribbling, incomplete bladder emptying.
Investigations: PSA test, ultrasound, urine flow test, DRE.
Allopathy: Alpha-blockers (Tamsulosin), 5-alpha reductase inhibitors, surgery (TURP).
Homeopathy: Sabal serrulata, Conium, Chimaphila, Thuja.
Ayurveda: Varunadi kwath, Gokshuradi guggulu, Kanchanar guggulu.
Diet & Lifestyle: Include tomatoes, pumpkin seeds, flax seeds, green tea. Avoid spicy food, caffeine, alcohol. Do pelvic floor exercises.
Benign Prostatic Hyperplasia (BPH)
Understanding Benign Prostatic Hyperplasia
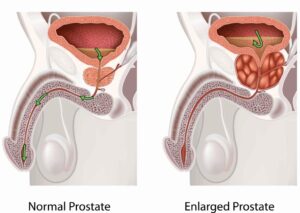
Benign Prostatic Hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland that commonly affects men as they age.
The prostate surrounds the urethra—the tube that carries urine out of the body. When the gland enlarges, it can press on the urethra and interfere with normal urination, leading to uncomfortable urinary symptoms.
BPH is very common—affecting nearly half of men over age 50—and while it’s not cancer, it can significantly impact quality of life if left untreated.
Causes and Risk Factors
The exact cause of prostate enlargement is not fully understood, but it’s strongly linked to hormonal changes that occur with aging.
Common risk factors include:
-
Age over 50
-
Family history of prostate problems
-
Hormonal imbalances (especially testosterone and estrogen changes)
-
Obesity or sedentary lifestyle
-
Diabetes and heart disease
Symptoms of BPH
As the prostate grows, it gradually blocks urine flow. Symptoms often develop slowly and may include:
-
Frequent urination, especially at night (nocturia)
-
Difficulty starting urination
-
Weak or interrupted urine stream
-
Feeling of incomplete bladder emptying
-
Urgency or leaking (dribbling) after urination
-
Pain or discomfort during urination (less common)
If untreated, severe cases may lead to urinary retention, bladder infections, or kidney problems.
When to See a Doctor
You should schedule an evaluation if you experience:
-
Trouble urinating or starting your flow
-
Frequent nighttime urination
-
Sudden inability to urinate (medical emergency)
-
Blood in the urine
-
Pain or burning during urination
Early diagnosis allows for easier, less invasive treatment and helps prevent complications.
Diagnosis
Your healthcare provider will perform a thorough evaluation, which may include:
-
Physical examination (including digital rectal exam)
-
Urine tests to rule out infection or other issues
-
Blood tests, including PSA (prostate-specific antigen)
-
Ultrasound or imaging of the bladder and prostate
-
Uroflowmetry (to measure urine flow strength)
These tests help determine the size of your prostate and how much it’s affecting your urinary tract.
Treatment Options for BPH
Treatment depends on the severity of your symptoms and how much they affect daily life.
1. Watchful Waiting (Active Monitoring)
For mild symptoms, your doctor may recommend monitoring your condition with lifestyle adjustments such as:
-
Reducing caffeine and alcohol intake
-
Avoiding fluids before bedtime
-
Exercising regularly
-
Managing weight and diet
2. Medications
Several prescription medications can help relieve symptoms:
-
Alpha-blockers (e.g., tamsulosin, alfuzosin) relax the muscles in the prostate and bladder neck.
-
5-alpha-reductase inhibitors (e.g., finasteride, dutasteride) shrink the prostate over time.
-
Sometimes, combination therapy is used for better results.
3. Minimally Invasive Treatments
When medications aren’t effective, advanced techniques can reduce prostate tissue and relieve pressure, including:
-
UroLift® System – lifts and holds the enlarged prostate tissue out of the way.
-
Rezum™ Water Vapor Therapy – uses steam to shrink excess prostate tissue.
-
Transurethral Microwave or Needle Ablation (TUMT/TUNA) – heat-based treatments to remove tissue.
4. Surgical Options
For severe cases, surgery may be recommended:
-
TURP (Transurethral Resection of the Prostate) – removes part of the prostate through the urethra.
-
Laser therapy – vaporizes or removes obstructive tissue with precision and minimal bleeding.
Your urologist will recommend the best treatment option based on your prostate size, symptoms, and overall health.
Living with BPH
With proper care, men with BPH can lead comfortable, active lives. Managing symptoms may include:
-
Staying hydrated but limiting fluids before bedtime
-
Avoiding bladder irritants (caffeine, alcohol, spicy foods)
-
Regular exercise to support urinary function
-
Following up with your doctor for routine prostate checks
